nalco group
bone, muscle & joint pain physio
BOOK NOW / WHATSAPP ABOUT YOUR PAIN OR INJURY
- ORCHARD 400 Orchard Road #12-12 Singapore 238875
- TAMPINES 9 Tampines Grande #01-20 Singapore 528735
- SERANGOON 265 Serangoon Central Drive #04-269 Singapore 550265
Home > Blog > Physiotherapy > Shoulder Physio > Conditions > Adhesive Capsulitis (Frozen Shoulder) Physiotherapy
Adhesive Capsulitis (Frozen Shoulder) Physiotherapy
Often called a stiff shoulder or “frozen shoulder,” adhesive capsulitis occurs in about 2% to 5% of the population. Typically it happens to women more than men and is typically usually in patients over the age of 45.
Of the people who have had adhesive capsulitis in 1 shoulder, unfortunately about 20-30% of them will develop frozen shoulder in the other shoulder as well.
What our senior physiotherapists do is to help patients with adhesive capsulitis
- decrease/treat pain and
stiffness in the affected shoulder joint
- restore shoulder movement in the safest and most effective way possible
What is Frozen Shoulder (Adhesive Capsulitis)?
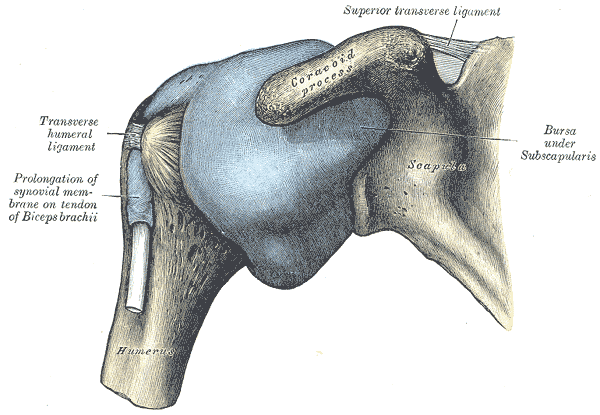
Adhesive capsulitis is the stiffening of the shoulder (and the shoulder joint) due to formation and thickening of scar tissue, which causes painful shoulder movement and decreased range of motion in the shoulder.
Unfortunately, research hadn't confirmed what's the actual conclusive causes of frozen shoulder, and the debate is that it's caused by either:
- Inflammation eg lining of a joint becomes inflamed (synovitis)
- Autoimmune reactions, where the body launches an "attack" against its own substances and tissues.
- Reactions after an injury or surgery
- Pain from other conditions, such as arthritis, a rotator cuff tear, bursitis, or tendinitis, that has caused a person to stop moving the shoulder
- Immobilization of the arm, such as in a sling, after surgery or fracture
what does frozen shoulder feel like?
Most people with adhesive capsulitis have progressively worsening pain and a loss of movement. Frozen shoulder can be broken down into 4 stages and our senior physiotherapist can help determine what stage you are in.
Stage 1: "Prefreezing" Stage
During stage 1 of its development, it may be difficult to identify your problem as adhesive capsulitis.
You've may have shoulder pain and stiffness symptoms for 1 to 3 months, and they seem to be getting worse. Any forms of movement of the shoulder causes pain.Your shoulder aches even when you're not using it, but the pain increases and becomes "sharper" with movement (especially movement with weights/resistance eg carrying a bag).
You may start to unconsciously protect your shoulder by decreasing the use and movement of the painful shoulder (this is normal). Mostly, the movement loss is most noticeable in "external rotation" (this is when you rotate your arm away from your body), but you might start to lose motion when you raise your arm or reach behind your back.
Pain is the #1 feature of this stage; and unfortunately you may experience shoulder pain during day and at night.
Stage 2: "Freezing" Stage
By this stage, you may have frozen shoulder symptoms for 3 to 9 months. You are also most likely have had a progressive loss of shoulder movement and an increase in shoulder pain (especially at night).
Your shoulder still has some range of movement, but it is limited by both pain and stiffness.
Stage 3: "Frozen" Stage
Your frozen shoulder symptoms have persisted for 9 to 14 months, and by now you may have greatly decreased range of shoulder movement. During the early part of this stage, there is still a substantial amount of pain but toward the end of this stage, the shoulder pain decreases, and the pain usually occurring only when you move your shoulder as far you can move it.
Stage 4: "Thawing" Stage
You've had symptoms for 12 to 15 months, and there is a big decrease in pain, especially at night. You still have a limited range of movement, but your ability to complete your daily activities involving overhead motion is improving at a rapid rate.
How Is frozen shoulder Diagnosed?
Unfortunately, most of the patients with frozen shoulder doesn't come to us until they're well into the 2nd or 3rd stage, and it's not surprising because most of the time, patients don't know that their shoulder pain is signs and symptoms of frozen shoulder.
Most times, patients are busy with work, life, family, responsibilities, or they just didn't know, so they may just ignore the pain or at best pop some painkillers or try to sleep it off.
Thing is, pain isn't normal, and should be quickly assessed and quickly treated - the earlier any pain or stiffness is assessed and treated, the less time it takes for it to recover. Basically early treatment = quicker and fuller recovery.
Our senior physiotherapists will perform a thorough shoulder examination and evaluation, including an extensive health history, to rule out other diagnoses.
Then they will look for a specific patterns in your shoulder's decreased range of motion called a "capsular pattern" that is typical with frozen shoulder. In addition, we have to also consider other conditions you might have, such as
- diabetes
- thyroid disorders
- autoimmune disorders
that are associated with adhesive capsulitis.
how our senior physiotherapists can help

Our physiotherapist's overall goal is to restore your movement, so you can
- go back to work
- go back to life and play
- go back to responsibilities
- go back to full movement and freedom without fear of shoulder pain
Once the evaluation process has identified the stage of your condition, our senior physiotherapist will create an individualized exercise program tailored to your specific needs. Exercise has been found to be most effective for those who are in stage 2 or higher. Your treatment may include:
Stages 1 and 2
Exercises and manual therapy. Our senior physiotherapist will help you maintain as much range of motion as possible and will help reduce your pain. They may use a combination of range-of-motion exercises and manual therapy (hands-on) techniques to maintain shoulder movement.
Modalities. Your physical therapist may use heat therapy and cold therapy treatments (modalities) to help relax the muscles prior to other forms of treatment.
Our senior physiotherapists will also match your physiotherapy treatment activities and intensity to your frozen shoulder symptoms, and educate you on appropriate use of the affected arm. Your therapist will carefully monitor your progress to ensure a safe healing procedure is followed.
Pain medication. Sometimes, conservative care cannot reduce the pain of adhesive capsulitis. In that case, your physical therapist may refer you for an injection of a safe anti-inflammatory and pain-relieving medication. Research has shown that although these injections don’t provide longer-term benefits for range of motion and don’t shorten the duration of the condition, they do offer short-term pain reduction.
Stage 3
The focus of treatment during phase 3 is on the return of motion. Treatment may include:
Stretching techniques. Our senior physiotherapist may introduce more intense stretching techniques to encourage greater movement and flexibility.
Manual therapy. We will increase your manual therapy to a higher level, encouraging the muscles and tissues to loosen up.
Strengthening exercises. You may begin strengthening exercises targeting the shoulder area as well as your core muscles. Your home-exercise program will change to include these exercises.
Stage 4
In the final stage, your physical therapist will focus on the return of "normal" shoulder body mechanics and your return to normal, everyday, pain-free activities. Your treatment may include:
Stretching techniques. The stretching techniques in this stage will be similar to previous ones you’ve learned, but will focus on the specific directions and positions that are limited for you.
Manual therapy. Manual therapy techniques in very specific positions and ranges that are problematic for you. They will focus on eliminating the last of your shoulder tightness and any residual limitations.
Strength training. Our senior physios will prescribe specific strengthening exercises related to any weakness that you may have to help you perform your work or recreational tasks.
Return to work or sport. We will address movements and tasks that are required in your daily and recreational life.
