nalco group
bone, muscle & joint pain physio
BOOK NOW / WHATSAPP ABOUT YOUR PAIN OR INJURY
- ORCHARD 400 Orchard Road #12-12 Singapore 238875
- TAMPINES 9 Tampines Grande #01-20 Singapore 528735
- SERANGOON 265 Serangoon Central Drive #04-269 Singapore 550265
Home > Blog > Physiotherapy > Conditions > Knee Pain > Plica Syndrome Physiotherapy
Plica Syndrome Physiotherapy

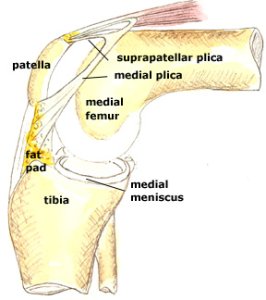
Plica syndrome is a type of painful knee condition and refers to an irritation of a small portion of tissue in the knee joint that is part of the joint capsule (synovial membrane).
Our synovial membrane produces fluid that helps to keep the knee joint lubricated. When this tissue on the inside of the kneecap becomes irritated, it results in knee pain and tenderness to touch.
Plca syndrome is often caused by repetitive trauma and overuse, though it also may result from a direct-hit injury. Plica syndrome is most often treated by our senior physiotherapists with the goals to
- improve mobility
- strengthening at the knee to decrease tension and irritation
What is Plica Syndrome?
Plica syndrome is an irritation of a portion of the synovial membrane in the knee. The synovial membrane encloses the knee joint and contains the fluid that keeps the joint lubricated.
Plica syndrome results when the synovial lining becomes irritated, typically the result of repetitive friction to the tissue, or in some cases a direct hit to the knee that traumatizes the tissue.
What happens is then this tissue will become thick, swollen and painful.
Repetitive friction is usually due to abnormal forces at the knee, most likely in the kneecap and surrounding musculature, or may be caused by muscular weaknesses or structural abnormalities at the hip or foot, which place increased tension on the knee. Of course, plica syndrome can also be caused or aggravated by increased activities.
Plica syndrome may result from a combination of several different factors, including:
- Decreased mobility of the kneecap
- Quadricep (front of the thigh) muscle or hip muscle tightness
- Muscular imbalances in the quadricep
- Muscular imbalances in the hamstring (back of the thigh)
- Muscular imbalances in the hip muscles
- Improper technique with repetitive activities
- Change in an exercise routine or sport activity
- Abnormal hip or knee structure
- Abnormal hip or knee mechanics
- Injury
How Does plica syndrome Feel like?
People with plica syndrome may experience:
- Pain and tenderness to touch in the front of the knee, and on the inside of the kneecap
- A "catching" or "snapping" sensation when bending the knee
- Dull knee pain at rest, which increases with activity
- Tightness in the knee
How Is It Diagnosed?
Our senior physiotherapists will review your medical history and complete a thorough examination of your knee. The goals of the initial examination are to assess the degree of the injury and determine the cause and contributing factors to your injury.
We will assess the mobility and strength of both lower extremities, including your foot and ankle as well as your knee and hip. Most often we will be able to feel a thickened piece of irritated tissue on your knee.
It is also common for us to perform a movement assessment, which may include
- watching you walk
- step onto a stair
- squat or
- balance on one leg
We also may ask questions about your daily activities, exercise regimens, and footwear to identify other contributing factors.
Imaging techniques, such as X-ray or MRI, are often not requested for, at least in the early or beginning stage. In the case of persistent pain, your doctor may decide to obtain an MRI to help identify the source of your pain.
Whether your pain was caused by a single injury or repetitive irritation, your initial examination as well as treatment will be similar. Initially, the primary goals are to calm down the inflamed tissue.
We will then address any underlying issues that may cause continued tissue irritation.
how our senior physiotherapists can help you
We will work together to develop a plan to achieve your specific goals. To do so, we will select treatment strategies in any or all of the following areas:
Pain Relief
Many pain-relief physiotherapy strategies may be implemented, such as applying cold therapy to the area or using therapies like iontophoresis (a medicated patch placed on the skin that is electrically charged and used to decrease pain and inflammation).
We will work with you to reduce your pain as much as possible without the use of pain medication, including opioids. We may also use
- ultrasound therapy
- radio-frequency Indiba physiotherapy
- dry needling
- stretching exercises
- joint mobilization
to help accelerate healing and decrease pain.
Range of motion
Your knee, hip, or foot may be moving improperly, causing increased strain at the front of the knee.
Self-stretching and manual therapy techniques (massage and movement) applied to the lower body to help restore and normalize motion in the knee, hip, and foot can decrease this tension.
Manual therapy
We may apply hands-on manual therapy treatments to move your muscles and joints in order to improve their motion and strength, most likely in your knee and hip. These techniques often address areas that are difficult to treat on your own.
Muscle strength.
Muscular weaknesses or imbalances can result in abnormal forces being applied to the front of the knee.
Based on your specific condition, we will design a safe, individualized, progressive resistance program for you, likely including your core (midsection) and lower extremities, and concentrating on the muscles surrounding the hip and knee.
These exercises may be completed in different positions such as lying down, sitting, or standing. We will choose what exercises are right for you, based on your age and physical condition.

Once your pain, strength, and motion improve, you will need to safely transition back into more demanding activities. To minimize the tension on the knee and your risk of repeated injury, it is important to teach your body safe, controlled movements.
Based on your goals and movement assessment, we will create a series of activities that will help you learn how to use and move your body correctly to safely perform the tasks required to achieve your goals.
Physical therapy promotes recovery from plica syndrome by addressing all contributing factors, such as
- pain
- any lack of strength, flexibility, or body control
We also may recommend a period of relative rest, then carefully guide your progression back to normal activity levels.
When Surgery Is Required
If your plica syndrome pain does not improve following several weeks of physical therapy with us, then arthroscopic surgery may be required.
Your surgeon will make small incisions in the front of the knee and remove the irritated tissue. Following surgery, your initial post-surgery physiotherapy with us will focus on
- decreasing pain
- restoring mobility
- restoring strength
We will then address specific factors that caused your plica to become irritated, in order to minimize the risk of further injury. As you progress, we will help you systematically reintroduce activities, including
- stair climbing
- squatting and
- desired recreational
