nalco group
bone, muscle & joint pain physio
BOOK NOW / WHATSAPP ABOUT YOUR PAIN OR INJURY
- ORCHARD 400 Orchard Road #12-12 Singapore 238875
- TAMPINES 9 Tampines Grande #01-20 Singapore 528735
- SERANGOON 265 Serangoon Central Drive #04-269 Singapore 550265
Home > Blog > Physiotherapy Singapore & Hand Therapy > Conditions > Spinal Pain > Spondylolisthesis Spinal Physio Singapore
Spondylolisthesis Spinal Physio Singapore
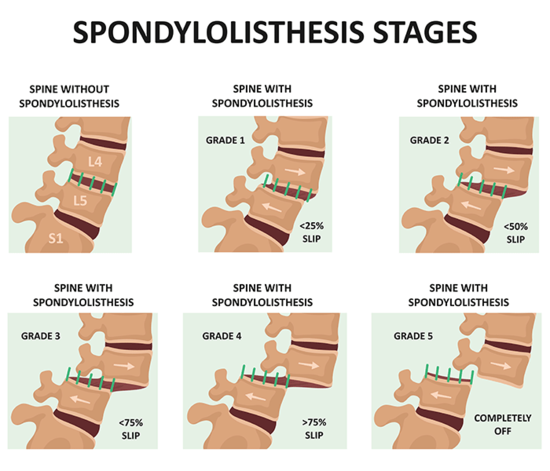
Image origin: https://www.nyp.org/ochspine/spondylolisthesis/treatment
Spondylolisthesis refers to a condition where the vertebral body (spine bone) "slips" move forward downwards in front of the vertebra below.
It's caused mainly by
- structural changes
- degenerative changes
- spinal fractures or
- sports activities that require a lot of spinal hyperextension and rotation
These causes fall into 2 different camps:
- isthmic most frequently in pre-teens and adolescents
- degenerative more commonly with aging and wear-and-tear over time
Spondylolisthesis diagnosis is usually made with a combination of
- medical history review
- physical examination
- imaging tests
and the severity of the vertebral slippage is graded from a scale from I to V, the higher / bigger the number = more severe.
What are the common Symptoms of Spondylolisthesis?
As spondylolisthesis worsens, patients will get more symptoms and / or worse symptoms such as
- Low back pain that gradually develops and worsens
- Specific pain in the buttock or leg
- Pain whenever they arch their back
- More and more swaying back of their sitting or standing posture
- Tight hamstring muscles (muscles at the back of the thighs, occurs in 80% of cases)
- Limp while walking
In moderate to severe cases, patients may also experience nerve or neurological symptoms, such as
- Numbness
- Tingling
- Burning
- Pins and needles
- Sciatica discomfort and pain
- Weakness in the leg
- Muscle tightness
- Delayed or decreased reflexes
In some cases, there may be visible or palpable "step deformity" (like a small bump or elevation) where the spondylolisthesis is.
first of all, What Causes a Spondylolisthesis?
As I shared earlier, there are two factors that cause spondylolisthesis: isthmic versus degenerative.
- Isthmic spondylolisthesis tends to be related to spondylolysis and occurs most frequently at the lumbosacral level (L5-S1) in more than 80% of the time.
- Degenerative spondylolisthesis on the other hand, happens mainly at the L4-L5 level (>88% of the time) and is usually related related to the degeneration of the posterior facet joints and intervertebral discs.
75% of the time, spondylolisthesis happens at L5-S1 and 20% happens at L4-L5. In some cases, it may be caused by a fall (which is pretty common in elderly or sporty individuals).
Other rare causes of spondylolisthesis:
- Dysplastic or congenital spondylolisthesis is caused by a poorly formed facet joint structure present at birth.
- Traumatic or pathological fractures and post-surgical failure.
Spondylolisthesis and it's relation to time / Age
- Congenital spondylolisthesis occurs when a baby's spine doesn't form the way it should before birth. The misaligned vertebrae put the person at risk for more chances of vertebral slippage later in life.
- Isthmic spondylolisthesis is most commonly seen in pre-teenagers and adolescents who play or are active in athletic activities that involve a lot of spinal hyperextension and rotation, such as gymnastics, cricket, hurdling, tennis, wrestling, and other racquet sports.
In such cases, spondylolysis (a back stress fracture) happens first and then it gradually worsens to the development of spondylolisthesis.
That being said, most cases of isthmic spondylolisthesis tend to stabilize after reaching skeletal maturity, and the fractures may not fully heal but are functionally controlled or balanced by the muscles which helps to prevent painful symptoms. - Degenerative spondylolisthesis, on the other hand, is a very common condition that is related to ageing, use and wear-and-tear. It is a natural phenomenon, and unfortunately most of us will possibly get this as we move about over time.
This type occurs due to chronic spinal segment instability caused by conditions such as degenerative disc disease or facet joint arthritis, and is more likely to cause recurrent symptoms and spinal stenosis, leading to gradual compromise of the spinal nerve roots, causing radicular pain syndrome or significant motor power deficits.
In severe cases, stenosis and slippage may compromise the cauda equina, a bundle of very important nerves at our tailbone, leading to cauda equina syndrome. This is dangerous situation and is medical emergency with immediate surgical intervention.
what are the risk factors to develop Spondylolisthesis?
- Individuals who are active or participate regularly in sports activities with a lot of spinal hyperextension and rotation, such as: gymnastics, tennis, cricket, wrestling, badminton
- Genetics: you have up to 26% probably of inheriting the condition from a parent.
- Ladies are up to 3X more likely to develop spondylolisthesis versus males who are up to 3X more likely to develop spondylosis without slippage.
- Global or generalized hypermobility ie increase "looseness" or range of motion in the joints
- Unusual or abnormalities in the share of the facet joints.
- Degenerative spondylolisthesis is more prevalent / common in pregnant women and black individuals.
- Spina bifida occulta, which is a congenital condition where the spinal bones don’t close completely around the spinal cord.
How to diagnose spinal Spondylolisthesis?
Here in Singapore, most of the time, the clinical diagnosis of spinal spondylolisthesis is done with a medical doctor or orthopedic surgeon, with
- medical history review
- symptoms interview
- physical assessment / examination which may involve checking for that step test, which is a noticeable step or depression in the back which can indicate positive for spondylolisthesis
- imaging tests such as x-rays, CT or MRI scans, are more detailed (MRI being the most clear and detailed) about any types of injuries such as fractures, pars defects, and degeneration in the vertebrae, discs, and facet joints. MRI scans can also help to rule out other potential causes of back pain, such as malignancy (tumours or cancers) or infections.
Spondylolisthesis Treatment
Majority of spondy
Treatment for spondylolisthesis typically starts with non-surgical methods. This may involve modifying activities and performing specific exercises prescribed by a physiotherapist. The prognosis for low-grade spondylolisthesis is generally good. However, the type of exercise performed can greatly impact the outcome. One study showed that one exercise group had a 73% improvement at three months compared to only a 33% improvement in the other exercise group. It is important to seek guidance from a physiotherapist for a personalised treatment plan and ensure that exercises are tailored to the individual’s spondylolisthesis.
Spondylolisthesis is graded on how far along the vertebral slippage has happened, with a grade from I to IV (the higher = the more severe or worse the slippage).
The grades are defined as follows:
- Grade I: 0-25% slippage
- Grade II: 25-50% slippage
- Grade III: 50-75% slippage
- Grade IV: 75-100% slippage
- Grade V: greater than 100% slippage (Spondyloptosis)
It is important to consult with a medical doctor or experienced physiotherapist for a proper diagnosis, grading, and appropriate medical and spinal physiotherapy treatment plan.
Physiotherapy Treatment
Physiotherapy treatments for spinal pains and spondylolisthesis will focus on
- pain relief
- managing muscle tightness and spasms
- increasing spinal stability
We may use a combination of
- Soft tissue management
- Cold therapy / Heat therapy
- Stretch therapy
- Strengthening
- Ultrasound therapy
- Shockwave therapy
- Mobilization of joints and tissues
- Dry needling
- Deep tissue release / massage treatment
- De-loading sports taping or supportive rigid taping
- Temporary mobility aids (orthotics, insoles, splints) to offload / support the injured and painful structures
- Exercise therapy
- Trigger point therapy
- Mobilization of joints and tissues
- Acupuncture
during the spinal physiotherapy sessions.
Specific spinal exercises are customized to activate and engage the deep stabilizing muscles in the spine that will both protect the spine's integrity and even help with posture and pain.
As your spondylolisthesis symptoms improve, we will continue to improve further your spine's strength, stamina and stability, with the goal to get you back to normal activities.
Spondylolisthesis chances of recovery (prognosis)
Most mild cases of spondylolisthesis is overall positive or favorable.
Patients with Grade I or II can expect improvements within a couple of physio sessions and the spine-strengthening and stabilizing exercises.
Only with very painful, unstable or severe grades (III and especially IV), or if there's loss of bladder or bowel function then patient may need to consider immediate surgery to do either
- spinal decompression surgery
- spinal fusion
Please make an appointment to see one of our spine physios and we can also refer you to a trustworthy spine doctor for first, second or even third opinion.
