nalco group
bone, muscle & joint pain physio
BOOK NOW / WHATSAPP ABOUT YOUR PAIN OR INJURY
- ORCHARD 400 Orchard Road #12-12 Singapore 238875
- TAMPINES 9 Tampines Grande #01-20 Singapore 528735
- SERANGOON 265 Serangoon Central Drive #04-269 Singapore 550265
Home > Blog > Physiotherapy > Conditions > Shoulder Pain > Left Shoulder Pain > Bankart Lesion Physiotherapy
Bankart Lesion Physiotherapy

A Bankart lesion (medically termed as a glenoid labrum tear), typically happens when the shoulder dislocates anteriorly (forwards), and this ends up damaging the lower part of the special cartilage that lines the shoulder socket.
Most of the time, it affects mainly young athletes.
Damage to the labrum makes the shoulder more risk to shoulder
instability and there is a high risk of further shoulder dislocation
without appropriate treatment.
Bankart lesions are named after English orthopedic surgeon Dr Arthur Sydney Blundell Bankart, who lived between 1879-1951, who first described the injury and the surgical repair process.
In this article we will look at the common causes, the associated injuries, the symptoms and the treatment options, both surgical and non surgical, for a typical Bankart lesion labrum tear.
first of all...What Causes A Bankart Lesion?
To fully understand Bankart lesions, we need to first understand the structure of the human shoulder.
Our shoulder is a ball and socket joint, similar to our hip joint. The top of the arm bone (head of the humerus) forms the "ball" part of the shoulder joint and the front part of the shoulder blade (glenoid fossa) forms the "socket" part of the joint.
To allow for the large range
of mobility that the shoulder needs to move the arm in multiple
directions, what ends up is that the socket part of the shoulder joint becomes/is very shallow.
To visualize, you can imagine by
- making a fist on your left hand
- use your right hand and place it over the first
You'd see that the joint is fairly shallow and can be easily dislocated/damaged.
Around the rim of the socket is
a special band of cartilage known as the glenoid labrum. This labrum is made
of fibrocartilaginous material and what it does is that specificly deepens the shoulder socket to improve
the connection of the joint and improving stability without compromising or restricting
mobility.
A Bankart lesion happens typically when there is damage to the lower portion of the glenoid labrum, causing it to break and tear away from the bony socket.
Usually this happens when the shoulder dislocates forward, meaning the head of the humerus is forced forwards and is pushed/popped out anteriorly of the glenoid socket.
As it is forced forwards, it will/may damage the labrum, causing it
to tear.
A vast majority of shoulder dislocations are anterior dislocations (over 95%) and are usually caused by:
1) Trauma
A fall onto an outstretched arm, particularly if the arm is
- abducted (stretched or extended out to the side)
- externally rotated (turned outwards away from the
body) and
- extended (behind)
This is the most common cause of anterior shoulder dislocations in older patients. Road traffic accidents (RTAs) are another cause of traumatic shoulder dislocations.
2) Sports And Sporting Injuries
Contact injuries such as football, soccer, water polo or rugby tackles, particularly when
the arm is above the head and the elbow is pushed backwards.

Repetitive
movements above the head such as
- cricket
- baseball
- tennis
- badminton
- swimming
can also cause this injury.
This is the most common cause of a glenoid labrum tear in younger and more active or sporty patients.
Associated and related shoulder Injuries
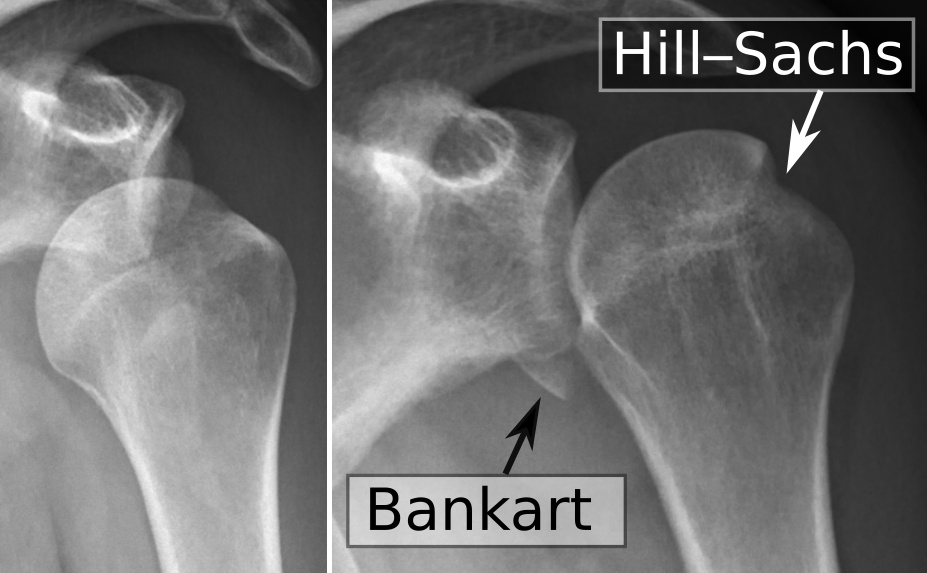
With forward anterior shoulder dislocations, on top of suffering from a labrum tear, in some cases, patients may also experience damage to one of the shoulder bones.
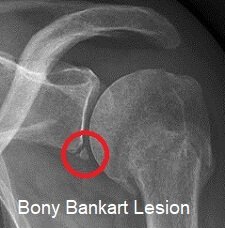
- Damage to the glenoid (the socket part) is known as a Bony Bankart. Bony Bankarts happen when there is a fracture (break) in the antero-inferior (lower front) part of the glenoid cavity, including the glenoid labrum tear.
- Bankart lesions may also be associated with fractures of the head of humerus (the ball), such as a Hill-Sachs lesion, where there is a compression fracture on the posterolateral (outer back) part of the humeral head.
- The joint capsule, a special sac that sounds the glenohumeral joint, may also be damaged, as may be the surrounding ligaments, most commonly the inferior glenohumeral ligament.
These all increase the risk of further shoulder instability.
Symptoms Of A Glenoid Labrum Tear

Common symptoms of a Bankart lesion include:
1) Recurrent Dislocations
Repeated episodes of shoulder dislocation are fairly common with a Bankart lesion, particularly in younger patients. It can affect up to 80% of people under the age of 30.
This frequency reduces with age to around 30% over time.
2) A Feeling of Looseness And/Or Instability
Patients report their shoulder may feel weak and as if it is going to dislocate again, with actions such as throwing or lifting and moving.
A common complaint is “my shoulder feels loose and can pop out any time or especially certain angle”
3) Pain
Our shoulder patients with a glenoid labrum tear often complain of an aching pain which tends to be diffuse (generalized pain over a location) rather than in one spot
4) Catching/Locking Sensations
Patients may experience unusual sensations when moving the arm with a labrum tear, such as tingling pain or burning sensations etc
bankart Treatment Options
There are two treatment options for Bankart lesions, surgical and
non-surgical. The right treatment will depend on factors such as severity, age,
activity levels and levels of instability.
1) Surgical Treatment
Surgery tends to be the treatment of choice for younger patients with a Bankart lesion, especially with patients who play sports, as there is a high risk of the shoulder dislocating again.
This is because the glenoid labrum tear often fails to heal properly, the reason is:
- labrum has poor blood supply, tends to heal slowly
- highly mobile area, so tends to reinjure
So when the glenoid labrum doesn’t provide the extra depth to the socket that is needed, it reduces the stability and increases the risk of further (recurrent) shoulder dislocation.
A Bankart lesion repair is usually carried out arthroscopically (hey hole surgery) under general anaesthetic. The labral tear surgery aims to repair and tighten overstretched and damaged
- ligaments
- joint capsule and
- cartilage
Suture anchors are placed in the bone and the torn glenoid labrum is
reattached to the glenoid fossa. Typically patients can go home same-day or one day after shoulder surgery like this.
You will need to wear a protective sling, even when you sleep to protect the shoulder for the first few weeks and allow it to heal in the correct position.
Shoulder physical therapy with our senior physiotherapists will be started almost immediately to
- regain strength
- stability and
- movement
You will be given a shoulder exercise and rehab
program to follow, which gradually progresses to more challenging exercises over
time.
It usually takes around 4-6 months to recover completely and be able to return to contact sports.
Fortunately, Bankart shoulder repair surgery has an approximately 85-90% success rate, with most of our shoulder pain patients returning to their pre-injury activity levels.
Outcome tends to be slightly better
when surgery is carried out soon after the initial labrum tear, rather
than further down the line.
2) Non-Surgical Treatment
For older patients, or those who are less active, conservative non-surgical treatment is recommended for a Bankart lesion.
The painful shoulder and arm is immobilized in a sling for a few weeks, usually with the arm resting across the front of the body in internal rotation (turned inwards) and a small pillow under the armpit to hold the arm slightly away from the body (slight abduction).
Patients are then referred to our senior physiotherapists for intensive shoulder physical therapy to regain the
- strength
- stability and
- mobility
of the affected shoulder.
One of the problems with this treatment method is that in this rest position, the glenoid labrum tends to heal in slightly the wrong place, so the socket depth is reduced, making the shoulder more prone to recurrent dislocations.
Except for young athletes, the advice is often to try non-surgical therapy first. If the shoulder does re-dislocate, then corrective shoulder surgery would be advised.
- cold therapy
- heat therapy
- moist heat paraffin wax therapy
- radio-frequency Indiba physiotherapy to accelerate soft tissue healing
- joint mobilization
- stretching exercises
- strengthening exercises
- scar management
- hands on manipulation and mobilization (manual therapy)
- soft tissue management
- heat therapy and heat treatment and heat pack to relief tight muscles and joints
- ultrasound therapy to accelerate soft tissue healing
- exercise therapy
- acupuncture and/or dry needling
- deep tissue release
- and more
References
