nalco group
bone, muscle & joint pain physio
BOOK NOW / WHATSAPP ABOUT YOUR PAIN OR INJURY
- ORCHARD 400 Orchard Road #12-12 Singapore 238875
- TAMPINES 9 Tampines Grande #01-20 Singapore 528735
- SERANGOON 265 Serangoon Central Drive #04-269 Singapore 550265
Home > Blog > Hand Therapy & Customized Splinting > Finger, Hand, Wrist, Forearm & Elbow Conditions > Elbow Pain Hand Physiotherapy
painful elbow hand physiotherapy
Hand therapy and physiotherapy has an important role to play in the management of pain and dysfunction of and around the elbow joint.
Experienced hand therapists and physiotherapists have functional knowledge of the complicated 3-joint elbow complex as well as its associated elbow anatomy; because of this, we can apply this knowledge to the various structures around the elbow as well as distant from the elbow that can contribute to a person's symptoms.
Our principal hand therapists and principal physiotherapists will perform a detailed assessment of the elbow and identify all contributing factors as well as co-morbidities associated with the person's symptoms.
What this detailed assessment does is that it will help us develop a multi-modal and multi-disciplinary treatment approach that is individualised to the specific problems and contributing factors found in the assessment of the painful elbow.
The Complex Anatomy of the Elbow
So our human elbow joint is where the distal humerus meets the proximal radius and ulna bones.
It is known as a trochleogingylomoid joint as it can flex and extend as a hinge (ginglymoid) joint as well as pivot around an axis (trochoid motion) known as pronation and supination.
The elbow joint is an extremely congruent and stable joint...
...and due to the complexity of the elbow, even after mild or severe injury, our elbow is more prone to stiffness than instability.
our elbow joint
The elbow joint is generally consisting of the articulation or joints of three (3) different bones, which are the:
- humerus bone (bone of the upper arm)
- radius bone (the long bone of the forearm on the outer side)
- ulnar bone (the long bone of the forearm on the inner side)
They make two general joints:
Ulno-humeral Joint (Ulnar + Humerus Elbow Joint)
- The ulnohumeral hinge joint is responsible for elbow flexion (bending) and extension (straightening).
- The spool-shaped trochlea of the humerus articulates with the greater sigmoid arch of the proximal ulna.
Radiocapitellar Joint (Radius + Capitellum Elbow Joint)
- The radiocapitellar joint is where the radius (radial bone) and humerus join.
- It is partly responsible for pronation (turning palm to face down) and supination (turning palm to face up).
- The capitellum of the lateral distal humerus is a spherical structure onto which the concave surface of the proximal radial head articulates.
Proximal Radio-ulnar Joint (Radius + Ulnar Elbow Joint)
- The proximal radioulnar joint is a trochoid joint that mainly works / is for pronation or supination of the forearm.
- The peripheral edge of the radial head articulates with the radial notch of the ulna.
Carrying Angle
- The carrying angle is measured when the elbow is in full extension and full supination. It is an angle measured along the long axis of the humerus and ulna.
- Usually in men, it is approximately 11-14° and women 13-16°.
- In fact, this term "carrying angle" is appropriately named as it allows our arms to clear our hips as we walk and allows objects to be carried.
Movements of the Elbow
Flexion and Extension
Elbow flexion (bending) and extension (straightening) happens at the ulnohumeral joint. The normal range of movement is from 0-140° but note that "only" 30°-130° is required for most ADLs
Pronation and Supination
The radiocapitellar joint and proximal radioulnar joint are responsible for pronation and supination.
Normal ROM is considered approximately 180° (80°-90° pronation and 90° supination). 100° of movement (50° pronation and 50° supination) is considered adequate for most ADLs.
If pronation ROM is lost this can be compensated by using shoulder abduction.
But, there is no compensatory action for supination and as such a loss of supination ROM can pose a greater disability than a loss of pronation ROM.
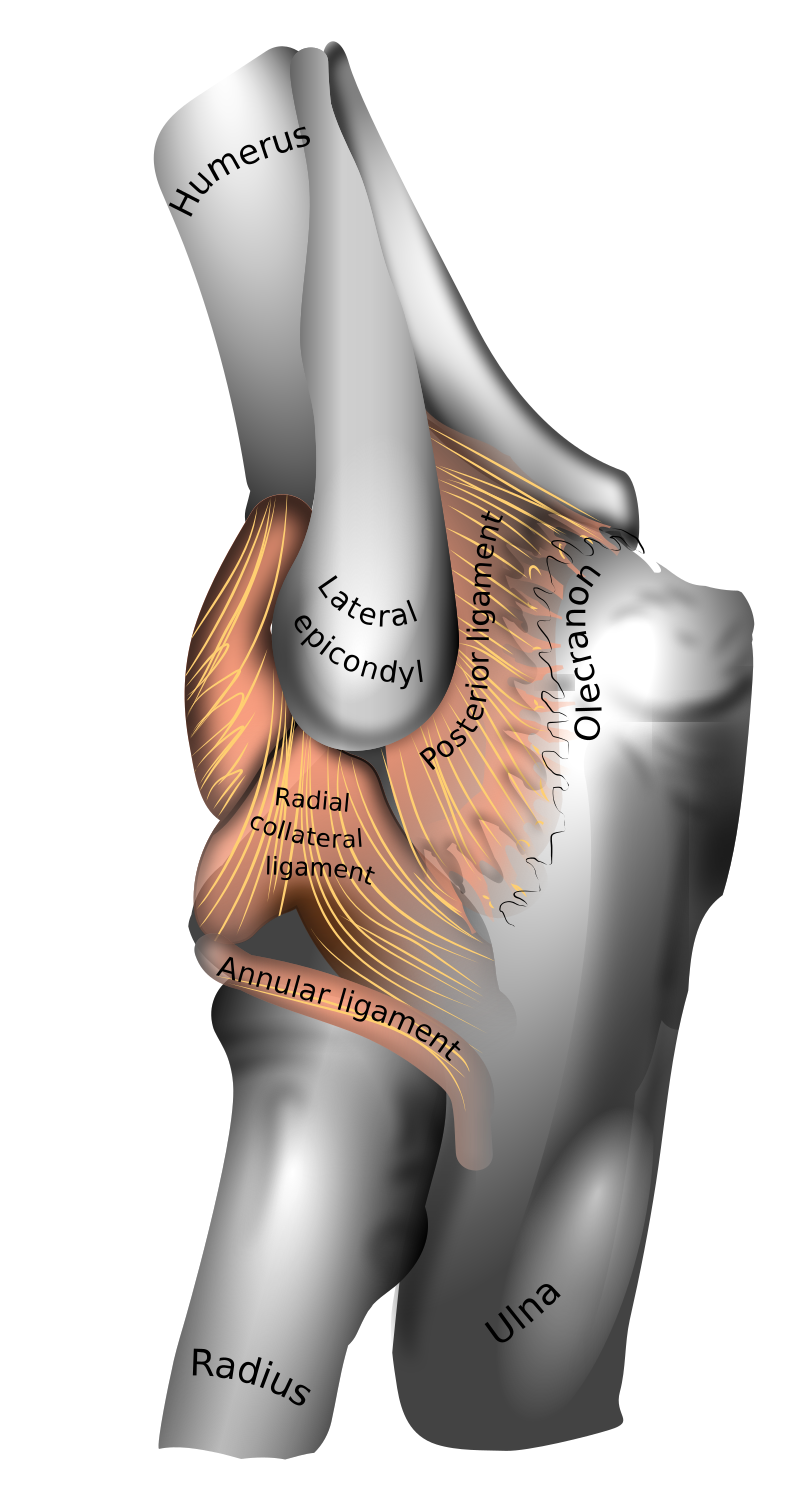
elbow Ligaments and Capsule
There are 2 main ligament complexes at the elbow namely the Medial and Lateral Collateral.
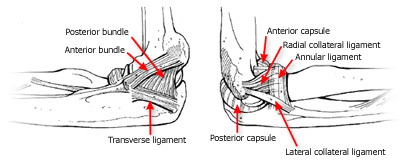
Elbow Medial Collateral Ligament Complex (MCLC)
The MCLC is comprised of the anterior bundle, posterior bundle and transverse ligament (the ligament of Cooper). The anterior bundle is considered to be the most important stabiliser of the elbow and provides valgus and posteromedial stability.
The anterior bundle is further divided into the anterior and posterior bands. The anterior band is more taught in extension and relaxes into flexion and the posterior band is taught in flexion and releases in extension.
This makes the anterior band more vulnerable to valgus stress when the elbow is extended and the posterior band of the AMCL more vulnerable to valgus stress when the elbow is flexed.
Elbow Lateral Collateral Ligament Complex (LCLC)
The LCLC is the primary stabiliser against varus and external rotation stresses. The lateral ulnar collateral ligament, the radial collateral ligament and the annular ligament form the LCLC.
The lateral ulnar collateral ligament is important in maintaining posterolateral rotatory stability as well as stabilising against varus stresses. The radial collateral ligament also contributes to posterolateral rotational stability.
The Annular ligament surrounds the radial head but does not attach to it. It is am important stabiliser of the proximal radioulnar and radiocapitellar joint.
Joint Capsule
The joint capsule of the elbow surrounds all 3 joints.
There are thickening medially and laterally of the joint capsule that blensd with the MCLC and LCLC respectively and contributes tothe stability of the elbow.
elbow Muscles
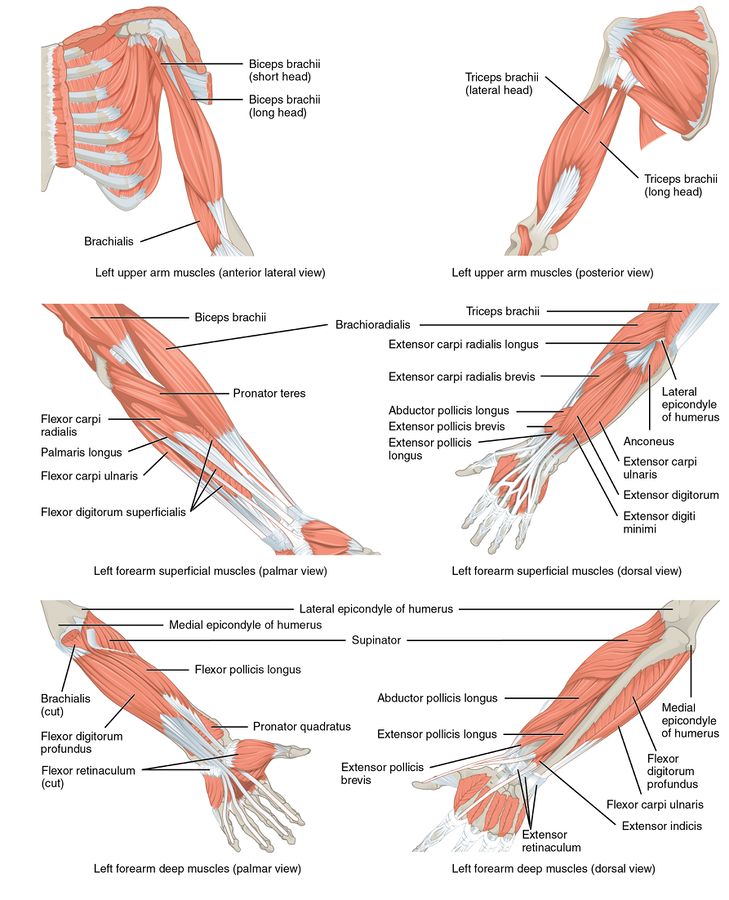
There are 4 main muscle groups at the elbow.
The anterior bicep group, the posterior tricep group, the lateral extensor-supinator group and the medial flexor-pronator group
Each muscle group applies a compressive load to the elbow joint when they contract.
Primary Elbow Flexors
- Brachialis
- Biceps brachii
- Brachioradialis
Secondary Elbow Flexors
- Pronator teres
- Extensor carpi radialis longus
- Flexor carpi radialis (at elbow angles 50 degrees or more)
Primary Elbow Extensors
- Triceps
- Anconeus
- Secondary extensors
- Flexor Carpi ulnaris
- Extensor carpi ulnaris
Pronation
- Pronator teres
- Pronator quadratus
Supination
- Mainly Biceps Assistance from supinator
- Lesser degree finger and wrist extensors
Differential Diagnosis of Elbow Pain
Statistically, lateral elbow pain (pain in the outer side of the elbow) is the most common site for pain to be felt at the elbow.
Lateral epicondylalgia or tennis elbow is a common cause of lateral elbow pain but it is not the only cause. There are many conditions that can cause pain and dysfunction at the elbow and a systematic differential diagnosis is important to identify all contributing and predisposing factors.
Anterior (Front) Elbow Conditions
- Biceps insertion tendinopathy rupture
- Brachialis Strain / Tear
- Degenerative Joint Changes
- Adult Annular Ligament Tear / Sprains
Medial (Innerside) Elbow Conditions
- Medial Epicondylalgia (golfer's elbow)
- MCL strain / rupture
- Ulnar Nerve Entrapments
- Medial olecranon fossa impingement
Lateral (Outerside) Elbow Conditions
- Lateral Epicondylalgia
- Osteochondral Fractures of the capitellum
- Osteochondritis Dissecans
- Synovial Plica
- LCL tear/ strain (also known as elbow ulnar collateral ligament strain)
- Fractures of the Radial Head
- Loose Bodies
- Osteoarthritis of the elbow radiohumeral joint
- Synovitis Radio-humeral joint
- Radial tunnel syndrome
- Posterior interosseous Nerve entrapment
Posterior (Back) Elbow Conditions
- Avulsion fractures of the olecranon
- Olecranon spurs
- Olecranon posterior impingement
- Triceps tendinopathy / Rupture
- Olecranon Bursitis
- Postero/lateral elbow dislocation
Factors Contributing to Elbow Pain
Elbow pain most of the time, does not occur in isolation ie it's not a standalone issue usually.
Many structures can refer pain to the elbow and others can contribute to the development of elbow pain and dysfunction. It has been shown in various studies that structures distant to the elbow contribute to the development of elbow pain and dysfunction.
These can be from a variety of dysfunctions namely
- neural, myofascial
- joint-related or even
- centrally mediated
Shoulder, Cervical Spine and Thoracic Spine
The cervical and thoracic spine have been shown to influence elbow pain.
In a study, by Berglund et al in (2008), 70% of subjects with lateral elbow pain also experienced pain in their cervical and thoracic region whereas the asymptomatic group only reported 16%.
Weakness of the scapular muscles, particularly serratus anterior as well as lower and middle traps, have been shown to be a significant risk factor in the development of elbow pathology.
Fatigue in these muscles can alter the biomechanics of upper limb activity and thereby cause dysfunction at the elbow.
A study conducted in 2012 by Lucado et al found that female tennis players with lateral epicondylalgia showed greater weakness in their wrist extensors and lower trapezius muscles compared to asymptomatic players.
This study contained a relatively small sample size and as such does not represent a direct causal relationship but rather factors to consider in the diagnosis and management of elbow pathology.
Compensatory movements at the elbow can occur as a result of dysfunction at other joint complexes in the body. An example being if there is a loss of glenohumeral lateral rotation range of motion there may be an increase in forearm supination or valgus as a compensatory strategy.
Alternatively, a loss of glenohumeral internal rotation range of motion may result in an increase in forearm pronation.
These compensatory movements can result in problems occurring at the various elbow structures. Treating the local elbow pain will not resolve symptoms as the primary problem of reduced shoulder mobility needs to be addressed to reduce the increased stress at the elbow.
The Role of the Central Nervous system
As in any pain condition, the central nervous system plays an important role in elbow pain and dysfunction. Depression and anxiety have been associated with upper extremity complaints and should be considered when managing elbow conditions.
Central sensitisation can be a cause of hyperalgesia and altered pain processing at the elbow. This centrally mediated process is important to identify as standard peripheral biomechanical based treatment may not be as effective in patients presenting with symptoms of central sensitisation.
Patients with central sensitisation potentially experience short-term and long-term pain as well as increased disability.
Cold hyperalgesia as a means of identifying central sensitisation in the elbow could be a useful diagnostic test to identify altered pain processing.
A study conducted by Maxwell and Sterling in 2013 on patients with neck pain showed that a Numeric Pain rating scale of greater than 5 after a 10-second application of ice to the neck is a good indicator of cold hyperalgesia.
Physiotherapy Management of Elbow Pain and Dysfunction
The management of lateral epicondylalgia has been well researched.
The other conditions found around the elbow have not been as widely researched and evidence-based practice for those conditions may be more focused on general clinical experience than on specific researched evidence.
It is well accepted that a comprehensive management programme of elbow pain and dysfunction requires a multi-modal approach. Active management of musculoskeletal pain disorders involving self-management is more supported by evidence than passive management strategies.
Treatment should be aimed not only at the local elbow structures found on assessment but at all the contributing factors identified during the examination.
There is moderate evidence that manual therapy can have immediate beneficial effects on pain and grip strength.
Mulligan mobilisations which are aimed at pain-free movement during a mobilization technique have been shown to be beneficial.
Manual therapy at the cervical and thoracic regions have also shown to provide clinical benefits in LET management
Exercise Therapy
Exercise therapy has the best evidence for good treatment outcomes in lateral epicondylalgia.
Optimal loads have not yet been established and various subgroups of patients may benefit from different loading strategies.
Isometrics may produce an analgesic effect and in general, exercises that are centred around loading the tendon should not aggravate the pain.
Tendon neuroplastic training
Tendon neuroplastic training as descrived by Rio et al has been shown to be an effective management programme for lower limb tendinopathies.
It has not been studied in upper limb tendinopathies in detail. Welsh (2018) published a case report with a TNT programme being applied to 2 separate patients with lateral elbow tendinopathy with promising results.
Electrotherapy including
- Ultrasound therapy to accelerate soft tissue healing
- Extracorporeal shockwave therapy
- NMES neuro-muscular electrical stimulation
- EMS electrical muscule stimulation
Stretching Therapy & Range of Motion
